The spine includes the cervical, thoracic, lumbosacral sections and is connected to a chain with 33-34 vertebrae located on top of each other.During daily physical activity, the spine has physiological (normal) curves to evenly distribute the load on the spine and when the body is in an upright position.In the cervical and lumbar regions (lordosis) and two convex in the thoracic and sacral regions, two curved convex convex (silkness).Between the vertebrae, there are intervertebral discs - cartilage, which performs the function of shock absorption and consists of the nucleus pulposus and a fibrous ring around it.
Spinal osteochondrosis is a chronic disease characterized by the development of degenerative-dystrophic changes in the intervertebral discs with subsequent involvement of adjacent vertebrae and surrounding tissues.
Currently, doctors more often use the broader term "dorsopathy" to replace the concept of "dorsopathy", sometimes "osteochondrosis".Dorsopathy neck (cervicalgia), neck and head (cervicokraticji), neck and shoulders (cervicobrachialgia), chest pain (lumbodni), back pain (lumbodynia), back pain (lumbodni), back pain (lumbodynia), back pain (lumbodynia), back pain (lumbodynia), back pain (lumbodynia), pain in the back (lumbodynia), back pain (Lumbodni), back pain (Lumbodni), pain in the back (Lumbodynia), back pain (Lumbodni),including back pain.
Causes of spinal osteochondrosis
To date, there is no accurate information about the causes of degenerative changes in the back.There are a number of theories that take into account various factors: participation (participation - reverse development, retrograde movement), mechanical, immune, hormonal, dysmetabolic, vascular, infectious, functional and hereditary.The most common, working theory, is that premature aging of this or previous (local) cartilage and bone occurs as a result of previous mechanical or inflammatory damage.According to this theory, the development of degenerative changes in the spine is genetically predetermined, and the occurrence of the disease with corresponding clinical manifestations is related to the influence of various endogenous (internal) and exogenous (external) factors.
The probability of osteochondrosis increases with age, excess weight, a sedentary lifestyle and poor physical fitness, on the one hand, and exposure to heavy physical work and vibration, on the other hand
The load on the spine increases in proportion to the increase in body weight, so overweight people suffer from overload even under conditions of moderate activity;The condition predisposes to physical inactivity due to poor tolerance to physical activity.
Psycho-emotional stress combined with a sedentary lifestyle leads to tension in individual muscle groups, changes in muscle tone and movement patterns - posture, gait.The development of scoliosis - lateral curvature of the spine, pathological kyphosis and lordosis (aggravation of physiological curves) also contributes to the deformation of the intervertebral discs.
Disease classification
By placement:
- osteochondrosis of the cervical spine;
- osteochondrosis of the thoracic spine;
- Osteochondrosis of the lumbar and sacral spine.
According to the stage of the disease:
- exacerbation (maximum number of clinical manifestations);
- remission (absence of clinical manifestations).
Depending on which forms are pathologically affected, the affected structures of the spine differ:
- Reflex syndromes - reflex tension of innervated muscles or muscle tonic diseases (muscle spasms), developed when vascular, autonomic, dystrophic - pain receptors are irritated.
- Compression syndromes often involve a nerve root, spinal cord or vessel (radiculopathy, myelopathy, myelopathy, myelopathy, myelopathy, myolopathy, myelopathy, radiculoischemic syndrome are distinguished).
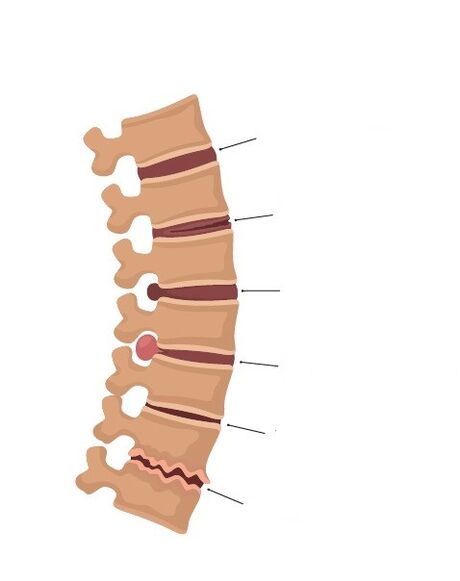
Depending on the stage of development of the process, there are:
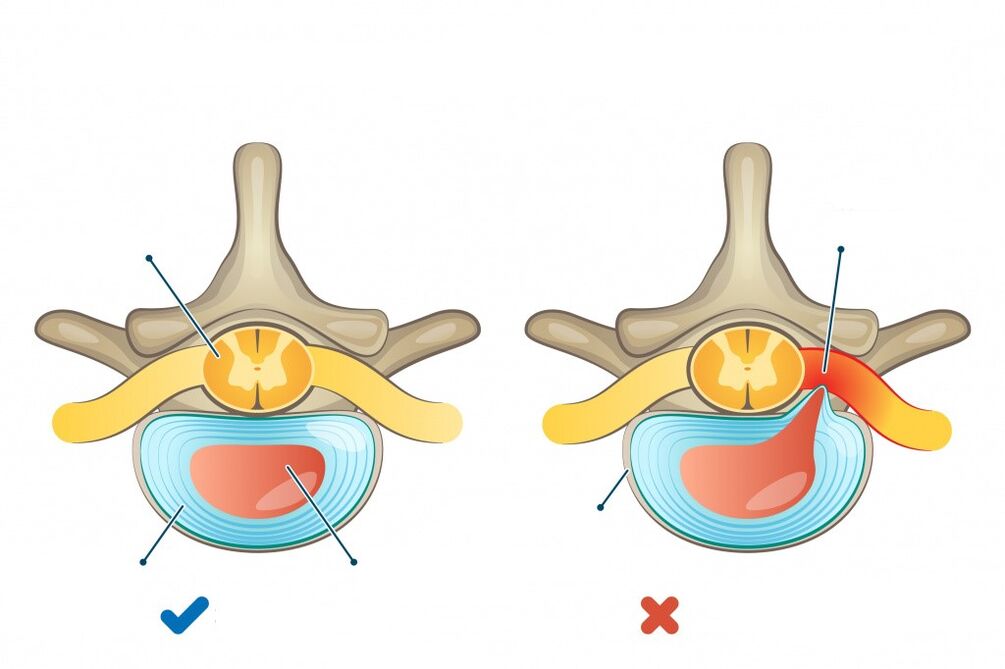
- Stage of intradiscal pathological process (chondrosis).During this period, the intradiscal movement of the nuclei pulposus occurs.The Nucleus Pulposus penetrates the outer fibers through fissures in the fibrous ring.As a result, nerve endings are irritated and pain develops.
- Stage of instability or when the affected disc is displaced relative to the base of the extreme vertebra.During this period, instability syndrome, reflex and even compression syndromes may occur.
- The stage of the formation of herniated intervertebral discs due to the violation of the integrity of the fibrous ring, which can compress the neighboring neural structures, including the root of the spine, the spinal nerve root.
- Stage of formation of fibrosis of intervertebral discs and marginal osteochondral enlargement of vertebral bodies, compensatory growth in the area of immobility of vertebrase and support in defective discs.In some cases, these bony growths can compress adjacent neural formations, such as disc herniations.
Symptoms of osteochondrosis
Symptoms of osteochondrosis depend on the area of damage to the spine and the degree of changes occurring in it, and the function of internal organs may be disturbed.
Osteochondrosis of the cervical spine is characterized by pain in the neck, aggravated by movement, accompanied by numbness in the arm and fingers.
Complaints of vision, dizziness, vertigo, tinnitus, darkening of the eyes or darkening of spots in front of the eyes are possible.
When affecting the thoracic spine, patients are in the heart region, long-lasting, painful or pressing, quite sharp, stabbing, sharply persistent.
When the arms are enlarged, sneezing, coughing, bending and turning of the body, deep breathing or strengthening can occur.There may be a feeling of numbness in the skin on the chest, abdomen and back.
Patients with osteochondrosis of the lumbosacral region note the stiffness of the movement, it is worse when walking, walking, lifting heavy objects, one or the other leg flutters.
Possible vegetative disorders: palatability of the skin of the feet, at a comfortable temperature for the rest of the legs.The skin of the legs and buttocks has a feeling of numbness, paresthesia (sensation of pins and needles).
Diagnosis of the disease
Instrumental Diagnostics includes x-rays of the spine to rule out traumatic injuries, congenital structural anomalies, and detect bony growths.The study is also carried out with functional tests - taking pictures during flexion and extension in the cervical and lumbar regions to rule out pathological displacement of the vertebrae relative to each other.






















